Latest evidence on Hospital in the home programs: implementation, sustainability and patient perspectives
Two companion Cochrane reviews and a new Cochrane Library editorial on Hospital at home programs were published this week. Here, Cochrane authors Dr Jason Wallis and Professor Sasha Shepperd share their key findings.
Hospital in the Home (HITH) programs have been on the rise in response to the COVID-19 pandemic
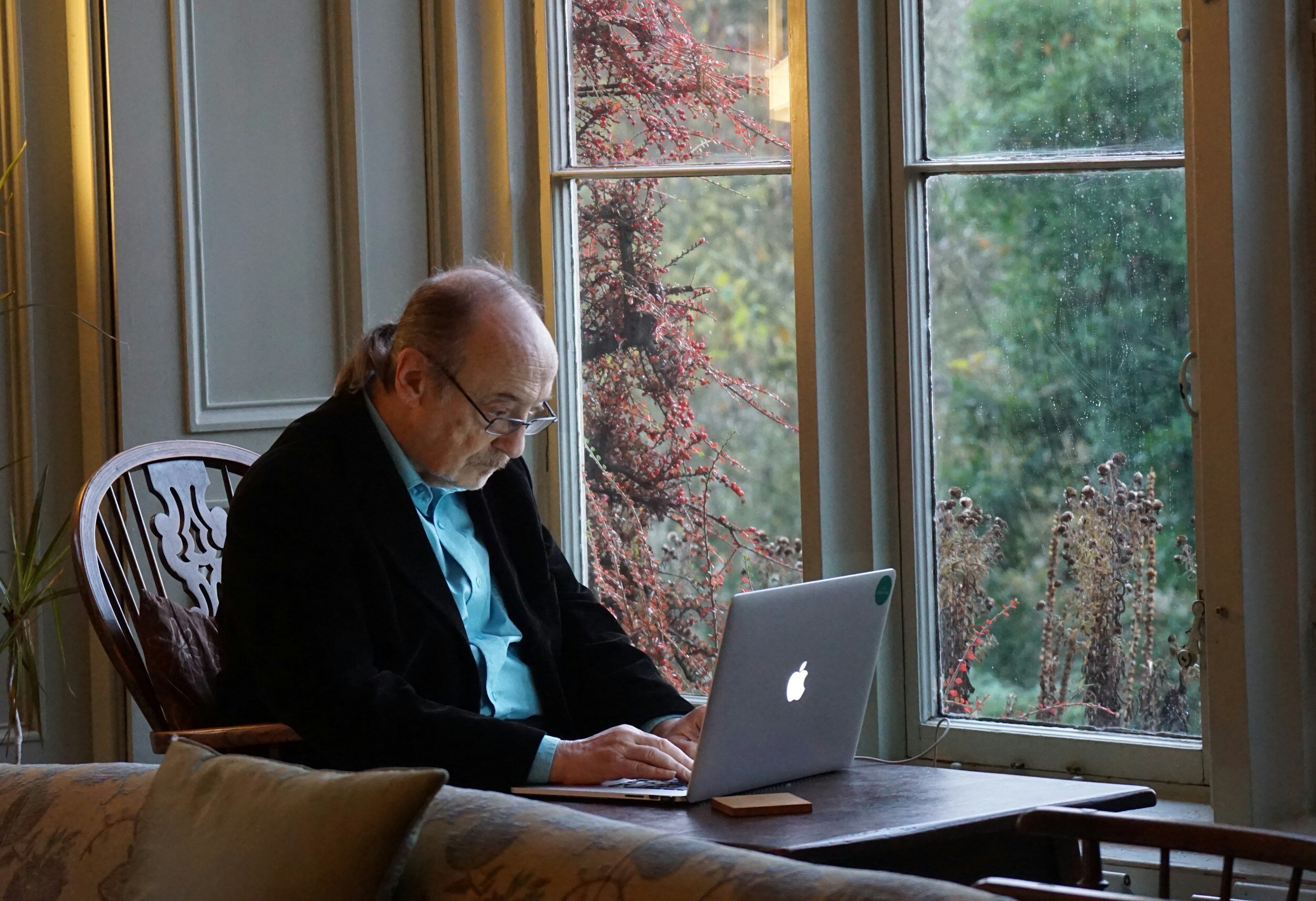
‘Hospital at home – or Hospital in the Home (HITH) as it’s better known here in Australia – is a service designed for people whose condition would normally need treatment in a hospital bed,’ explains Jason Wallis, researcher at Monash University’s School of Public Health. ‘Instead, with HITH they typically receive visits from a doctor, nurse and allied health professionals at home instead – just as they would if they were in hospital.’
‘We know there’s been a significant increase in HITH programs around the globe as an alternative to hospital admission, with more services being set-up during the COVID-19 pandemic to relieve the pressure on hospital beds and increase capacity. There are two types of programs. The first is called ‘admission avoidance’ as patients are referred by emergency doctors or general practitioners for HITH, thereby avoiding admission to a hospital ward. The other type is called ‘early discharge’ and is designed to shorten the length of time patients need to stay in hospital.’
‘While there’s a growing evidence base on both the effectiveness and cost‐effectiveness of both types of HITH programs, our review team recognised that health service managers, health professionals and policy makers need more evidence on how to actually implement and sustain these services on a wider scale. That’s why we undertook these reviews.’
What the latest evidence tells us…
Jason worked with Professor Sasha Shepperd and an international team of Cochrane researchers to analyse 52 qualitative studies from 13 countries that included interviews with over 2,000 people, including patients with a variety of conditions such as stroke or pneumonia, family caregivers, health professionals delivering or referring to HITH, as well as health managers and policy makers.
The review findings highlight several key areas for healthcare leaders to consider. These include the need to:
develop specific strategies to address specialists’ uncertainty about referrals to HITH and expand routes of referral
deliver more and better training to expand the roles of staff and increase the capacity for medical care in the home
focus on better recognising and defining the unpaid caregivers’ role, and providing support to unpaid caregivers
Financial barriers and questions around cost effectiveness
‘A range of barriers were identified across the studies we looked at,’ Jason says. ‘One of the most critical issues was a reluctance of some hospital specialists to refer patients to the HITH services, and their difficulty with identifying eligible patients. Early engagement with hospital specialists and emergency physicians who refer the patients, and providing clear eligibility criteria for referring patients are key to addressing this problem. It’s essential to build trust and understanding so clinicians become comfortable referring patients to HITH programs.’
‘Financial barriers were also a key challenge. Though we know from previous research that it can be cheaper to treat someone at home rather than in hospital, policy makers and hospital finance teams need clear evidence of financial benefit, or at least that the program doesn’t actually cost more. Some services found it very difficult to measure the financial impact of HITH programs for their respective hospitals – particularly private hospitals that had multiple payers with different reimbursement schedules to deal with. Some overcame this by starting small with a limited number of eligible patients before expanding.’
The update of the admission avoidance HITH included 20 studies, of these 12 reported cost data. In general, HITH appeared less costly than hospital, ‘but this is uncertain due to a range of different methods used to calculate cost, different unit costs and follow-up times.’
Other key themes: effectiveness, safety and patient perspectives
‘We were keen to include clinician, patient and carer perspectives in our research,’ Jason says. ‘We found that safety was the primary concern for patients considering having hospital at home. For example, many patients were concerned about being alone and not having the round the clock staff supervision that they would have in a hospital bed. On the other hand, there were also privacy concerns with patients not wanting staff in their homes.’
‘The impact of HITH on the caregiver was really interesting and quite mixed. While the impact could be positive – for example they didn’t have to travel to see their loved one in hospital – there was also this negative impact. Many carers reported feeling stressed, unsupported, unpaid and suffering from disruptions to their sleep and usual work routines.’
‘Few studies reported on patient satisfaction and as is often the case, data on length of stay varied among trials,’ Sasha adds. ‘Overall in terms of effectiveness, while few studies reported on adverse events, we’re moderately confident that admission avoidance hospital at home doesn’t make a difference to the number of older people who died when compared to in-hospital care. Similarly, we’re moderately confident that at six months follow-up the risk of a new admission to residential care was reduced for an older population who were allocated to hospital at home rather than admission to hospital.’
Next steps
‘While additional large randomised trials that include an analysis of cost-effectiveness will add to the certainty of the evidence’ Sasha concludes, ‘the lack of effective scaling‐up strategies means future research should also investigate the degree to which HITH substitutes for hospital based care and how HITH can be more widely implemented in a way that supports unpaid caregivers without creating additional work.’
‘As the Cochrane Library editorial published today alongside our reviews highlights, the critical need now is to identify and test strategies that can increase the adoption, uptake and sustainability of HITH programs across different healthcare systems – including strategies for engagement of referrers, patients and caregivers, and strategies for process optimisation and sustainability.’
‘This transition in research focus is critical for HITH to be a core part of every acute hospital's care strategy and extend its impact to transform patient care on a larger scale.’
Download this review social media tile to share